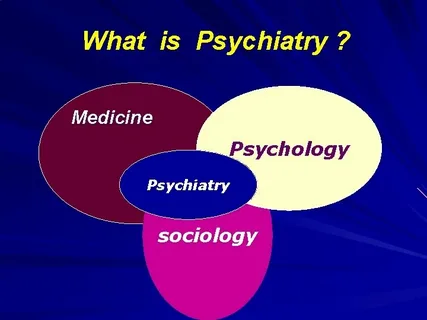
Psychiatry is the branch of medicine focused on the diagnosis, treatment, and prevention of mental, emotional, and behavioral disorders. Unlike other mental health disciplines, psychiatry is firmly rooted in the medical tradition. A psychiatrist is a medical doctor (M.D. or D.O.) who specializes in mental health, including substance use disorders. This medical foundation is crucial because it allows these specialists to understand the intricate relationship between physical and mental health, recognizing that emotional struggles often have biological underpinnings and systemic physical consequences.
The field has evolved significantly from its early days, moving away from purely abstract theories of the mind toward a rigorous, evidence-based understanding of brain chemistry, genetics, and neurobiology. Institutions like Liv Hospital are at the forefront of this modern approach, employing a biopsychosocial model that views mental health through the lens of biological factors, psychological influences, and social environmental contexts.
The Scope of Psychiatric Conditions
The range of conditions treated within psychiatry is vast, covering everything from temporary emotional distress to chronic, lifelong conditions. These disorders can significantly disrupt a person’s thinking, feeling, mood, and ability to relate to others.
Mood Disorders are among the most common reasons individuals seek psychiatric help. This category includes Major Depressive Disorder, characterized by persistent sadness and a loss of interest in daily activities, and Bipolar Disorder, which involves distinct episodes of mania (high energy/euphoria) and depression. These are not merely “bad moods” but are linked to imbalances in neurotransmitters, the brain’s chemical messengers such as serotonin, norepinephrine, and dopamine.
Anxiety Disorders go beyond normal stress or worry. Conditions like Generalized Anxiety Disorder (GAD), Panic Disorder, and Social Anxiety Disorder involve excessive, uncontrollable fear and anxiety that interfere with daily functioning. The physiological response in these conditions—rapid heart rate, sweating, and hyperventilation—demonstrates the deep connection between the brain’s alarm systems and the body’s physical state.
Psychotic Disorders, such as Schizophrenia, involve a disconnection from reality. Symptoms may include hallucinations (hearing or seeing things that aren’t there) and delusions (false beliefs). These conditions often require complex medical management to stabilize brain chemistry and restore functional capacity.
Neurodevelopmental Disorders, including Attention-Deficit/Hyperactivity Disorder (ADHD) and Autism Spectrum Disorder (ASD), are also within the purview of psychiatry. While often diagnosed in childhood, these conditions frequently persist into adulthood, requiring ongoing management and adaptation strategies.
The Diagnostic Process
Diagnosing a psychiatric condition is a meticulous process. Unlike a simple blood test for high cholesterol, there is no single biological marker for most mental disorders. Instead, psychiatrists rely on comprehensive clinical evaluations. This involves a detailed interview about symptoms, personal and family medical history, and the progression of the condition.
Crucially, because psychiatrists are physicians, they can order and interpret a full range of medical laboratory tests and imaging studies. This is vital to rule out physical causes for mental symptoms. For example, a thyroid imbalance can mimic depression, and a vitamin deficiency might present as fatigue or cognitive decline. By ensuring the diagnosis is accurate, the medical team avoids treating a symptom while missing the underlying cause.
Treatment Modalities: A Multidimensional Approach
Once a diagnosis is established, the treatment plan is tailored to the individual. Modern psychiatry rarely relies on a single method; instead, it combines therapies for maximum efficacy.
Psychopharmacology is the use of medications to treat mental disorders. Antidepressants, antipsychotics, mood stabilizers, and anxiolytics are prescribed to correct chemical imbalances in the brain. For instance, Selective Serotonin Reuptake Inhibitors (SSRIs) increase the availability of serotonin in the brain, helping to alleviate symptoms of depression and anxiety. The management of these medications requires careful monitoring to balance efficacy with potential side effects.
Psychotherapy, often referred to as talk therapy, is frequently used in conjunction with medication. Cognitive Behavioral Therapy (CBT), for example, helps patients identify and change negative thought patterns and behaviors. While psychologists and therapists often deliver these treatments, psychiatrists are trained in various psychotherapeutic modalities and may provide therapy themselves or coordinate closely with a therapy team.
Interventional Psychiatry represents the cutting edge of the field. For treatment-resistant conditions, advanced techniques such as Transcranial Magnetic Stimulation (TMS) or Electroconvulsive Therapy (ECT) may be employed. These therapies directly modulate brain activity to relieve symptoms when medication alone has proven insufficient.
The Importance of Specialized Care
Mental health is dynamic. A treatment that works today may need adjustment tomorrow. The department ofPSYCHIATRY ensures that patients receive continuous, adaptive care. Specialists monitor how a patient responds to treatment, adjusting dosages or changing medications as needed. This ongoing relationship is essential for managing chronic conditions and preventing relapse.
Furthermore, the integration of psychiatry into general healthcare is critical. Mental health disorders increase the risk of physical health problems such as heart disease, diabetes, and stroke. Conversely, chronic physical illness can increase the risk of mental illness. A specialized psychiatric team works in concert with other medical departments to ensure the patient is treated as a whole person, not just a collection of symptoms.
Recovery and management of mental health issues extend beyond the clinic and the pharmacy. While medical intervention corrects biological imbalances and therapy addresses psychological patterns, the environment and lifestyle of the patient play a massive role in sustaining long-term mental health. Sleep hygiene, nutritional balance, physical activity, and stress management techniques are not just supplementary; they are foundational to the success of psychiatric treatment. For those looking to integrate these broader wellness strategies into their daily routine alongside their medical care, resources likelive and feel can provide guidance on cultivating a lifestyle that supports mental and emotional resilience. Combining professional medical treatment with proactive lifestyle management offers the most robust path toward stability and well-being.